Shiga toxin-producing E. coli (STEC) including E. coli O157:H7
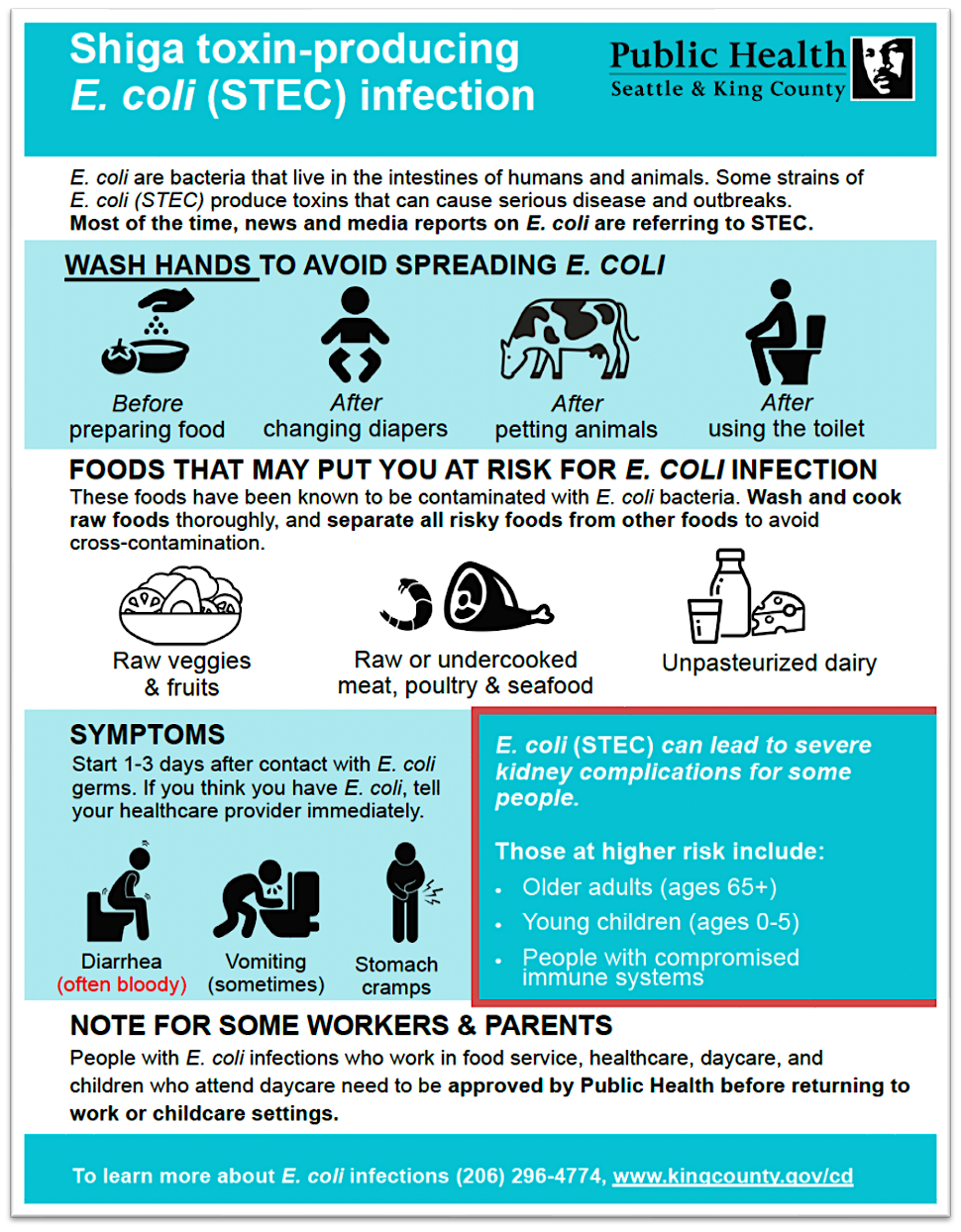
E. coli are bacteria that normally live in the intestines of humans and animals. Many strains of E. coli bacteria exist, and most of them are harmless or beneficial to human health. However, strains that produce Shiga toxin (such as E. coli O157:H7) can cause serious illness in people.
Symptoms typically appear one to ten days after exposure (usually within 2–4 days) and include: diarrhea (which often becomes bloody) and stomach cramps, with mild or no fever. Up to 15% of cases can develop a kidney complication called hemolytic uremic syndrome (HUS); children under the age of five are particularly affected. Shiga toxin-producing E. coli (STEC) infections are diagnosed by doing special tests on a stool sample from an ill person.
Infection with STEC can occur through consumption of: undercooked ground beef and other beef products; unpasteurized milk, cheese, and juice; contaminated raw fruits, vegetables, and herbs; water contaminated with animal feces, or by direct contact with farm animals or their environment. Ready-to-eat foods can also be contaminated with STEC through contact with raw beef or raw beef juices in the kitchen. Large multi-state outbreaks involving commercially distributed food products including beef, produce, and cheese have occurred in recent years.
Person-to-person transmission of E. coli can occur through the fecal-oral route, including transmission within households, child day-care centers, and long-term care facilities. Transmission is facilitated by inadequate hand washing after a bowel movement and contamination of objects in the environment.
Resources for the general public
- E. coli facts, CDC
- Health risks from consuming raw (unpasteurized) milk and milk products
- Biosolid recycling and E. coli
Resources for health care professionals
- E. coli guidance for healthcare providers and clinical laboratories, CDC
- Recommendations for Diagnosis of Shiga Toxin-Producing Escherichia coli Infections by Clinical Laboratories, MMWR, CDC
- Shiga toxin-producing E. coli infection (including but not limited to E. coli 0157:H7) is a reportable condition in King County: See disease reporting requirements.

 Translate
Translate