Hepatitis A
Hepatitis A virus infects the liver and can cause illnesses that range from a mild infection that has no symptoms to a more severe illness that can last for months. In rare occasions, it can cause liver failure and death.
Hepatitis A virus spreads easily. It gets into the body through the mouth after someone touches an object, food, or drink that is contaminated with the virus.
If an infected person doesn’t wash their hands well, especially after using the toilet, undetectable amounts of the virus can spread from the hands of that person to other objects, surfaces, and foods.
Most cases occur through eating contaminated food.
On November 29, 2021, the WA State Dept. of Health and Public Health – Seattle & King County reported that the hepatitis A outbreak among people living homeless appeared to be over.
For more information, please visit:
People at highest risk for getting hepatitis A
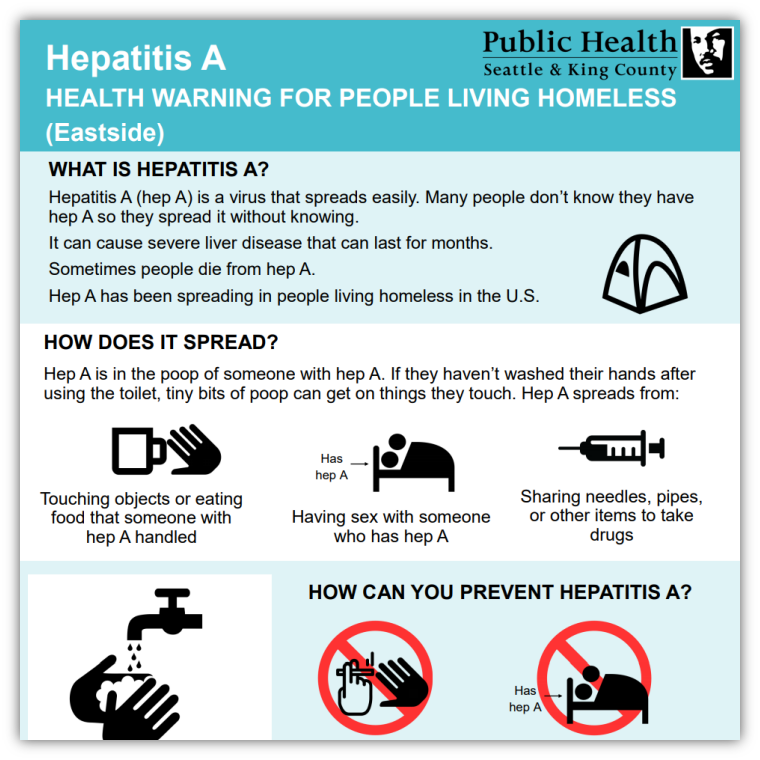
- People living homeless, especially those living unsheltered without good access to sanitation, hygiene and handwashing facilities
- People who are living with or caring for a person who already has hepatitis A
- People who have sex with people with hepatitis A
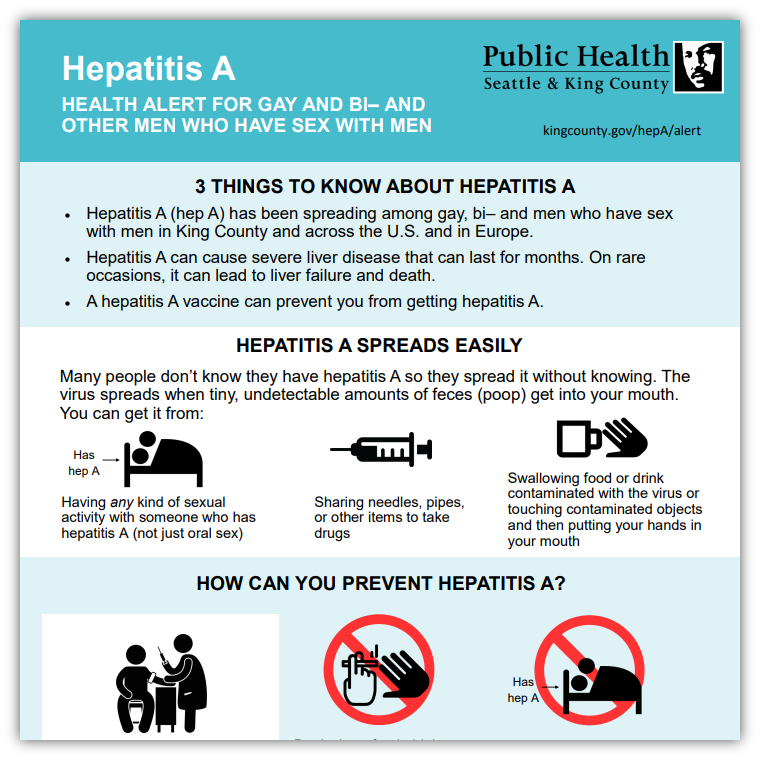
- Men who have sex with men
- People who use street drugs
- People with clotting disorders like hemophilia
- International travelers
- People with chronic liver disease, including hepatitis B and hepatitis C are at increased risk for severe infections
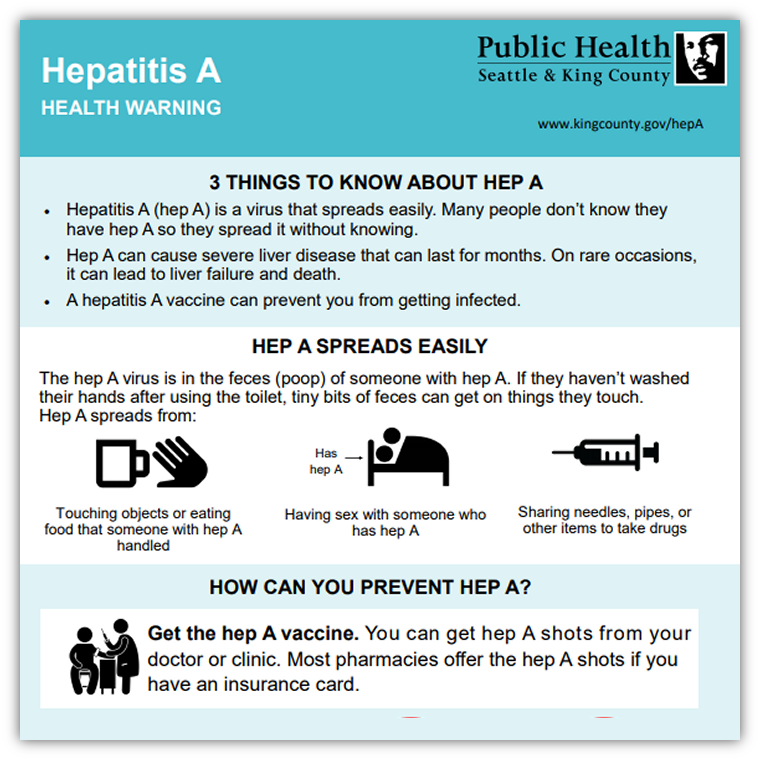
Hepatitis A Health Warning infographic for general public
Common symptoms include:
- Tiredness
- Nausea
- Vomiting
- abdominal pain
- loss of appetite
- low-grade fever
- yellow discoloration of the whites of the eyes and skin (jaundice)
- clay-colored bowel movements
- dark urine
- joint pain
Some people get infected with hepatitis A but do not experience all (or any) of these symptoms.
Hepatitis A vaccination is the best way to prevent hepatitis A. The shot is safe and effective; anyone who wants to reduce their risk of hepatitis A should get vaccinated. Anyone who is in the higher risk groups should be sure to get the hepatitis A vaccine to protect themselves.
Hepatitis A vaccinations can also be used to help prevent illness from hepatitis A among those who may have been exposed to the virus if given within two weeks of exposure.
Practicing good hand hygiene – including thoroughly washing hands after using the bathroom, changing diapers, and before preparing or eating food – also plays an important role in preventing the spread of hepatitis A. People in high risk groups should also avoid sharing food, drinks, drug equipment (works), and other personal items.
To get a hepatitis A vaccine, visit your doctor, nurse, or clinic. You can also check www.vaccinefinder.org for pharmacies that offer hepatitis A vaccine. Check our Healthcare for the Homeless Network page for information about vaccination locations for people living homeless or people who use street drugs.
Free hepatitis A vaccination locations for people living homeless
Hepatitis A: Health warning and free vaccine sites for people living homeless in:
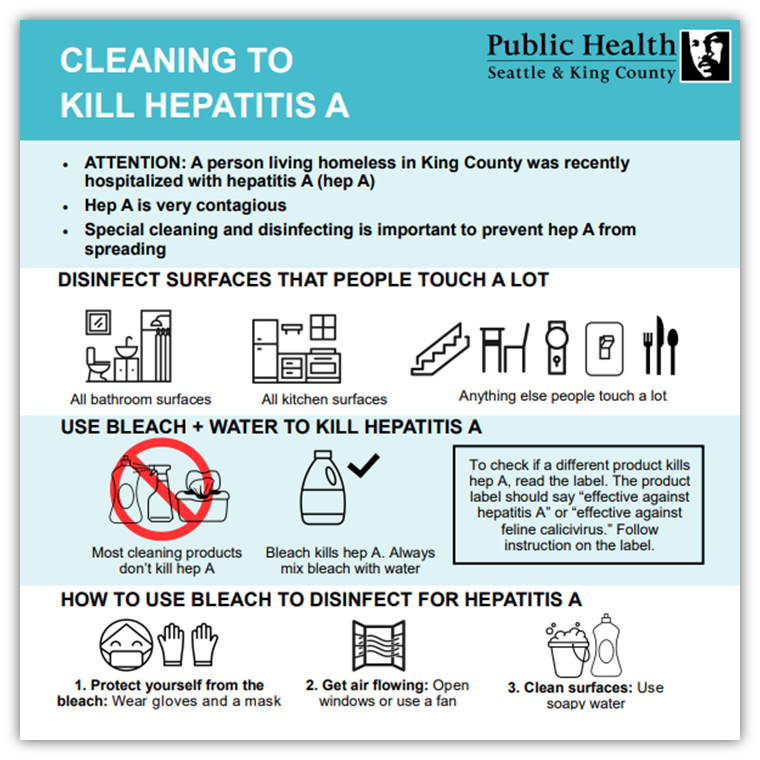
- Cleaning to kill Hepatitis A
Special cleaning and disinfecting is important to prevent hep A from spreading.
- ሄፓታይተስ ኤን ለመግደል ማጽዳት (Amharic)
- Nadiifinta lagu dilayo Cagaarshowga A (Somali)
- Limpieza para matar la hepatitis A (Spanish)
- Как проводить санобработку, чтобы уничтожить вирусы гепатита A (Russian)
- ጽሬት ንምቕታል ሄፓቲተስ A (Tigrinya)
- Chùi rửa sạch sẽ để tiêu diệt viêm gan A (Vietnamese)
- Routine cleaning guidelines
Homeless service provider agencies can also help prevent a major hepatitis A outbreak by making sure staff and clients are following routine cleaning guidelines.
Resources for health care professionals
Link/share our site at www.kingcounty.gov/hepa

 Translate
Translate